'Some days I despair that we're not making the progress we need,' says B.C. health officer of opioid crisis
Provincial health officer says addicts need easy access to safe pharmaceutical opioids
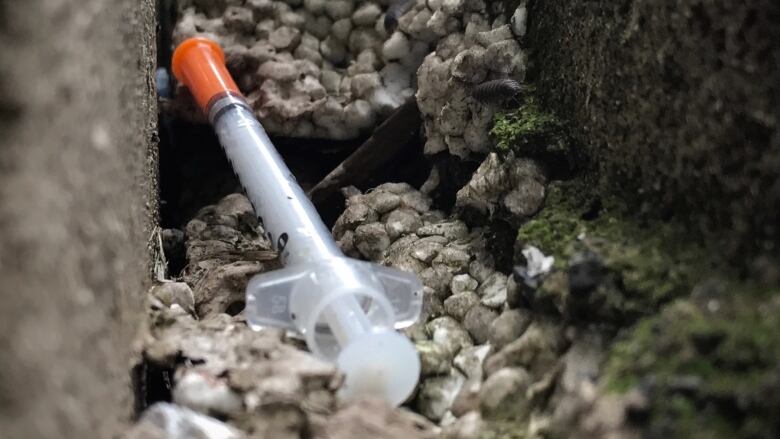
Despite the province's efforts, the number of people dying in B.C. from drug overdoses isn't decreasing.
In November, an average of four people died in B.C each day from drug overdoses, according to new numbers for the B.C. Coroners Service, with the death toll at 1,380 people between Jan. 1 and Nov. 30, 2018, nearly the same number recorded over the same period in 2017.
On the Coast guest host, Margaret Gallagher spoke with B.C.'s Health Officer Dr. Bonnie Henry about what steps the province is taking to tackle the crisis.

What do you think when you hear about the number of people who have died this year from drug overdoses?
It's incredibly discouraging. Some days I despair that we're not making the progress we need to make.
Why haven't we been able to slow the death toll, compared to 2017?
What's really been the driver of people dying here in B.C. is the toxicity of the street drug. If we had not put in place measures like distributing naloxone and [opening] supervised consumption sites, these numbers would be even higher, probably two-and-a-half to three times higher.
What can the province do to keep the drug supply safe?
Primarily, these are synthetic opioids imported from China, then mixed here with other toxic substances. One thing we can do is provide pharmaceutical opioids for people who have addictions to reduce their dependence on this toxic street drug.
What's being done to ensure access to safer substances?
We have a number of pilot projects where we provide [pharmaceutical opioids for] people who are dependent and need that daily fix.
[We are] looking at other low-barrier harm reduction approaches. The B.C. Centre for Diseases Control (CDC) is working on a project to provide a safe supply to people in supportive housing through the use of biometric machines for dispensing.
Vancouver's Overdose Emergency Task Force recommended that the city open a storefront space for a low-barrier hydromorphone dispersal pilot project. What are your thoughts?
I haven't seen the details, but that's exactly the type of thing we're looking at. This is not going to be the answer for everyone, but it will certainly make a difference for people who are dependent on this very toxic drug.
We don't hear much about the opioid crisis from the federal government. Why do you think that is?
It has been a challenge for us. They have expressed their support for us looking at ways of providing safer drug supplies.
But the other area I'm working very actively on is decriminalizing drug use. Making sure that we can take people who have addictions and who have this chronic relapsing disease and not put them in the criminal justice system, but divert them to places where they can get a safer supply and get connected to the support they need.
What are the chances we'll see fewer deaths in 2019?
I remain optimistic.
This interview has been edited for clarity; you can listen to it in its entirety below: